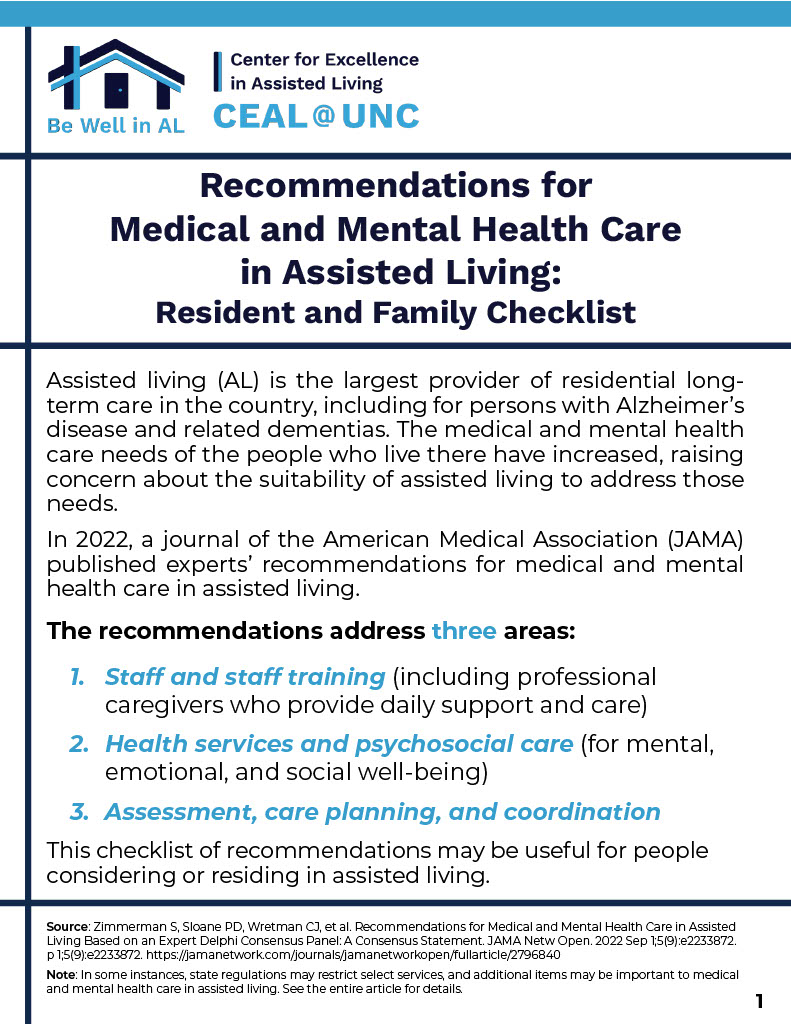
Dr. Sheryl Zimmerman, Executive Director of CEAL@UNC, is a guest columnist for McKnight’s Senior Living. These regularly published articles reflect the perspectives of CEAL@UNC advisors, and address timely topics relevant to the well-being of the people who live and work in assisted living. View Articles